Why are we making so little progress on Long COVID?
In February 2021 the federal government announced the “Researching COVID to Enhance Recovery” (RECOVER) initiative to tackle Long COVID. So far, $1.8 billion has been allocated to the program.1 It appears about $1.15 billion of that has been spent so far.2
Earlier this year I got an email from RECOVER commemorating the third anniversary of the program. Here’s how they characterized the impact so far:
Notice what’s missing? Treatments.
Why are we making so little progress? Well, a big part of the reason is that biomedical trials are very expensive and take a really long time to conduct. On the Institute for Progress website, Willy Chertman and Ruxandra Tesloianu published a list of possible reforms to address that problem.
There are other reasons though for the lack of progress, having to do with the complex nature of Long COVID:
Long COVID is defined in a really broad way
The standard definition for Long COVID boils down to “excess symptoms three months after a COVID-19 infection that are not attributable to any other cause.”
The SARS-CoV-2 virus can damage many parts of the body, leading to many possible mechanisms and symptoms.
Over 200 Long COVID symptoms have been reported, including, to name a few:
Loss of smell
Myocarditis
Atrial fibrulation
Shortness of breath
Tinnitus
Fatigue
Neuropathic pain
Believe it or not, the World Health Organization’s working group on defining Long COVID came up with an even broader definition. First, they decided that a positive test for COVID-19 isn’t necessary, only a “history of COVID-19”. Next, they decided that symptoms do not have to have started during or right after the acute phase of COVID-19 — they just have to have had a minimum duration of two months. In other words, it’s OK if patient’s symptoms started a month after COVID! A detailed study on adolescents found that, using the WHO’s definition, “acute COVID-19 was not an independent risk factor for Long COVID”. Check out the paper - it’s absurd!
There have been several papers that have tried to look at electronic health records (EHRs) and apply advanced clustering algorithms to identify a “Long COVID” cluster. Relatedly, some studies use machine learning to identify Long COVID patients from EHRs or blood biomarkers. I’m not sure these techniques help reduce the problem of false positives. More intriguing is using clustering to identify subclusters. A bunch of papers do this, and it appears there are some high-level clusters one can distinguish (like neurological, cardiopulmonary, etc).
False positives
Any symptom may be accidentally associated with COVID-19 due to temporal correlation. Fatigue, the most common Long COVID symptom, is extremely common and has numerous causes (at any given time, about 25% of people report suffering from fatigue). Samples of “Long COVID” patients may contain some false positives, where their symptoms are caused by something completely unrelated to their COVID infection. This makes doing research on the condition more difficult.
False negatives
False negatives are also possible. It’s easy for people to either not notice or be in denial about Long COVID symptoms. Based on experience interviewing over 200 people, Long COVID researcher David Putrino says that 25% of people who say they have recovered from COVID-19 actually have significant Long COVID symptoms upon further investigation. This seems really high to me, but it’s plausible. When conducting trials, careful screening of the control group is important for this reason.
Complexity.
Each person with Long COVID may have some or even all of these mechanisms causing their symptoms:
Organ damage
Blood-brain barrier damage
Epstein-Barr Reactivation
Persistent virus
Immune system dysfunction / autoimmune activation
Mitochondrial damage
Microclots (especially amyloid fibrin microclots)
False fatigue alarms generated by brain (aka a “faulty central governor”) or, more generally a type of functional neurological disorder causing fatigue
Autonomic nervous system dysfunction (POTS)
Depression (can be triggered by inflammation)
Anxiety (including health anxiety, somatization)
High stress (can cause fatigue, burnout)
Deconditioning (happens within a few weeks, much faster than people realize)
Sleep issues (for instance, being sick leads to a lot of time in bed which can upset Circardian rhythm leading to either insomnia or hypersomnia)
Symptoms from something else that are being mistakenly attributed to COVID-19 due to timing (false positive symptoms — this is super common)
Iatrogenic harm (ie from taking supplements, etc — also very common)
There is at least weak evidence for all of these, which you can verify for yourself via Google Scholar. There are additional proposed mechanisms which I feel skeptical about so I left them off the list: mast cell activation, cytomegalovirus reactivation, and microbiome disruption.
The relative proportions of these are not clear. My own suspicion is they are all roughly equally likely.
The fact there are many causal mechanisms and each patient may have one, two, or a even a dozen different causes is not something you hear widely discussed. Instead, researchers like to focus on a single cause and stake a claim that the causal mechanism they are studying is really important, perhaps even “the” cause for Long COVID.
There is a also a big split between people talking about brain-based mechanisms and “organic” mechanisms.3 The brain-based people insist it’s 100% brain-based, while the “organic” people insist it’s 100% organic. As Scott Alexander said a while ago, that’s not how any of this works. At the very least, all chronic conditions have a “psychosomatic shadow”.4
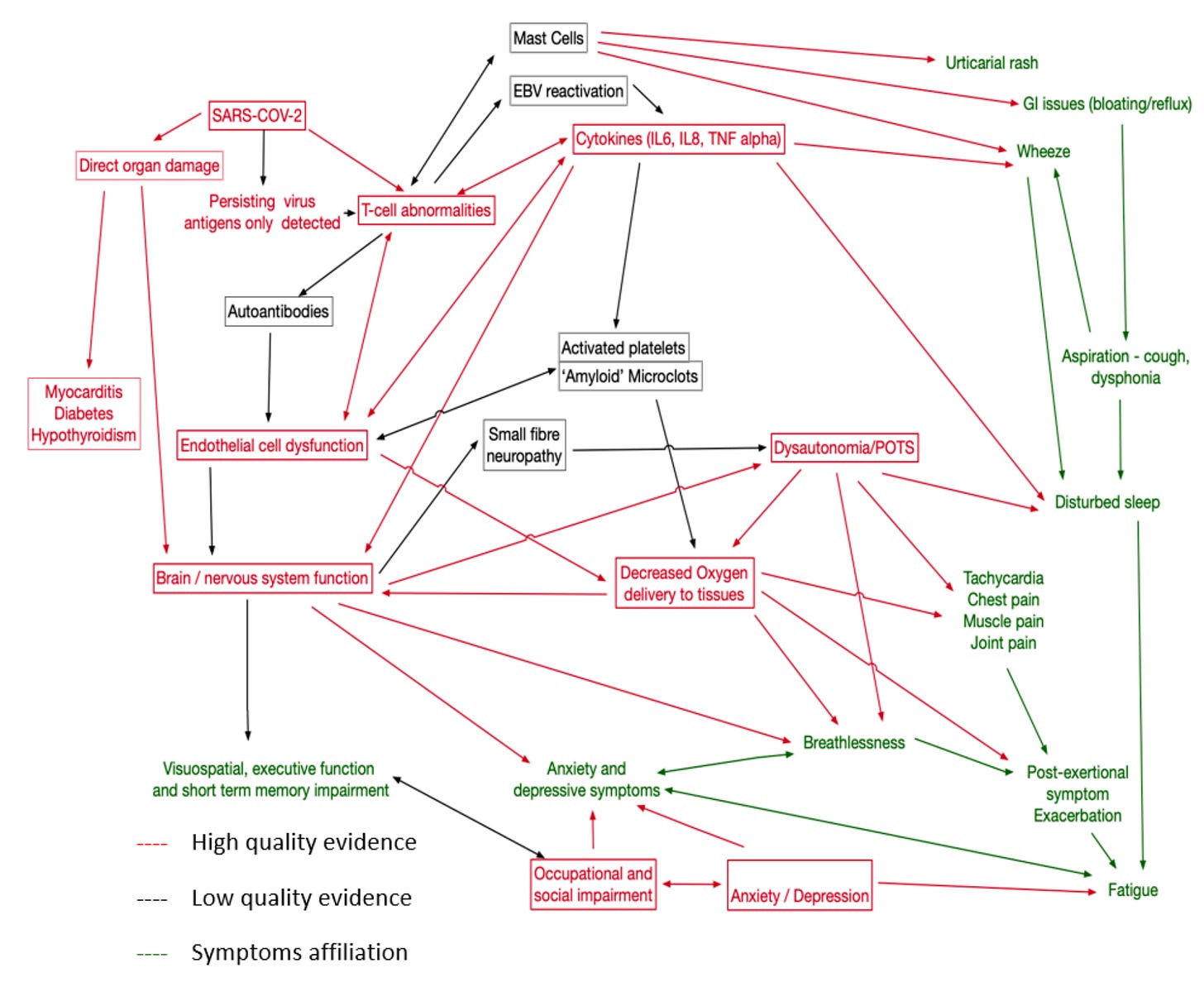
There are causal interconnections between a lot of these. Here’s one attempt to map out the causal web:
There are potentially causal arrows missing here — for instance some people think that inflammatory cytokines can cause depression.
The complexity of human health is astounding. A full understanding of the causal web for a complex chronic condition like Long COVID requires acknowledging that biological, neurological, psychological, and social-environmental factors all play a role and all feedback on each other (this is the biopychosocial model in a nutshell). Our biomedical research system is not well setup to handle complex bio-psycho-social conditions.
To think about this correctly, it’s also important to distinguish predisposing, precipitating, and perpetuating factors. A predisposing factor like depression might exacerbate Long COVID and make it harder to recover. Two months of persistent virus or Epstein-Barr reactivation might lead to the brain developing false fatigue alarms which becomes a perpetuating factor even after the Epstein-Barr reactivation has ended.
Anyway, the good news is I don’t think we have to fully understand this causal web to treat Long COVID. We only have to be able to identify the root mechanisms which are perpetuating the illness.
The other good news is that most of the things I listed above have established treatments. There is room for improvement in some areas, however. For instance, it appears there’s no cure for POTS, only band aid treatments that compensate for symptoms. Likewise, there’s no established treatment approach for “immune system dysfunction / autoimmune activation,” although there are a variety of drugs one can try.
It looks to me like the main difficulty here is figuring out which causal mechanisms any given person has.
How strategic was the RECOVER program? Did anyone roadmap this out?
Recently Adam Marblestone and others have been talking about how we don’t do enough strategic roadmapping in science. By roadmapping things out, we can identify bottlenecks to progress, whether they be scientific or institutional.
The RECOVER team apparently did some roadmapping. For instance, they decided to invest in infrastructure for biospecimen processing and data centralization. They also funded the RECOVER OMICS task force and research on “multi-omics” tools for Long COVID subtyping.
Speaking somewhat naively, I think a good initial investment would be to assemble a large sample of Long COVID patients and test them thoroughly to find the relative proportions for each of the key mechanisms listed above. Most of those mechanisms I listed were pretty obviously important by mid 2021, and some of them had been known to be implicated in other post-viral syndromes.
The only mechanism for which there is not a test is “false fatigue alarms”/“functional neurological disorder” - it remains a diagnosis of exclusion. There may be some types of immune dysfunction and autoimmune activation we don’t have tests for, as well.
To summarize how I conceive of everything personally:
It’s interesting to ponder the testing costs (I got these costs from ChatGPT and my own personal experience). Remember, a Long COVID patient may have some or even all of these problems. Testing for all would cost thousands of dollars!
It seems a good use of funds might be to invest in developing better testing technologies which are cheaper and more precise.
Going on a bit of an aside here, from a first principles perspective, there is no reason that medical imaging needs to be as expensive as it is. Of course, there is an initial fixed cost for the scanner. Then money is needed to pay for electricity to run the scanner. MRI cooling systems require regular maintenance and liquid helium top-off.
However, the main reason medical imaging costs so much is that technicians and clinicians have to be involved, and they require salaries and health insurance. The reason that MRI costs a lot more than CT is primarily that MRI scans take longer to run and technicians have to stand around that whole time.
A few years ago I had the idea of creating a “self serve MRI.” This is an MRI that is available 24/7 for anyone to use. An AI agent would instruct patients how to lie in the scanner and carry out the scanning protocol. For many things it’s possible to get away with the MRI being low-field, which would make it safe to bring metal into it (low-field MRIs should be cheaper to build too). AI could analyze all the images. In theory, there does not need to be a human in the loop.
MRI could look for organ damage in patients where it is suspected. It can also be used to gauge blood-brain barrier integrity, if a constrast agent is given.
PET scans to detect persistent virus is cool but probably there are cheaper methods. Naively, I think that persistent virus should leave some trace in the blood. Microfluidics combined with advanced immunological sensors might be the way to go.
As far as the tests for mitochondrial damage and microclots, I have no idea how those tests work. I hope someone is looking into why they cost so much.
Concluding thoughts
Building off the previous section, this is how I envision a strategic approach, at a high level:
Use testing to determine the prevalence of different disease mechanisms in the Long COVID population.
Strategically fund better testing technologies where it would be high impact to do so.
Using the initial results from 1., conduct large clinical trials that target specific mechanisms. Route patients to trials based on the mechanisms they have active, as revealed by testing.
RECOVER seems to be following this sort of strategy to some degree.
About 65% of the initial RECOVER funds went to “Clinical Research Studies.” It seems the bulk of that went to retrospective analyses and observational cohort studies. These studies often have many biases and tend to just document symptom prevalence and correlative risk factors. Some money went to autopsy studies and pathobiology studies, which are great since they illuminate mechanisms. Side note - for unknown reasons, the pathology study grants were recently terminated, but fortunately they were reinstated after an outcry was raised.
Out of the initial funding, only 15% went to randomized clinical trials. That’s not enough. Additionally, some of the trials are just putting band aids on, not treating mechanisms, in my view.5 Advocates are generally not happy with the selection of trials and some people think more experts on post-viral syndromes should have been consulted beforehand.
Globally, there are at least 100 active clinical trials studying Long COVID (see this table), and an additional 23 that have completed. About 9,000 articles have been published on Long COVID so far, and this number may double in the next year. I am currently working on having an LLM read as many of these as I can download. The LLM will be instructed to report back on the topics studied in each paper, what type of study it is, and the primary outcome of the study. With the help of the LLM, I’ll be able to create a comprehensive map of Long COVID research. Doing so should shed a lot more clarity on the overall situation.
In December 2020, Congress appropriated $1.15 billion to study Long COVID, leading to the formation of the RECOVER initiative in February 2021. Another $662 million was invested by congress into RECOVER in February 2024. This money was released in two tranches of $515 million and $147 million. According to an article from January, 2025, NIH is still “figuring out how to spend” that $662 million, $300 million of which has been earmarked for clinical trials. As a side note, Bernie Sanders wants the US government to spend $10 billion on Long COVID research over the next ten years. There is probably a good case for that, given the economic impacts of Long COVID. Planning has begun for the next phase of RECOVER, RECOVER-TLC, but it appears it has not been funded yet.
In July 2021, $860 million in COVID funds being administered by HHS were reallocated to cover medical costs for unaccompanied children at the Southern Border. According to the RECOVER program, “most of the funds” were transferred to the “Administration for Children and Families.” The RECOVER program casts what happened as a change in management, not a redirection of funds, and there were “no disruption of NIH activities.” Exactly what happened is very murky. I had ChatGPT do some Deep Research on this.
This should be clear, but “brain-based” includes the following phenomena - the way conscious thoughts and beliefs can create symptoms in the body and influence their perception, a faulty subconscious central governor that generates “false alarm” fatigue, and more broadly, other fringe theories about broken fatigue circuitry that fall under the “functional neurological disorder” umbrella. The size of the psychosomatic shadow for Long COVID is unknown, but it’s very unlikely to be close to zero. Additionally, patients with organic causes can also have psychosomatic effects as well — and in my experience people flinch away from acknowledging that extra complexity.
Scott uses the term “psychosomatic shadow” to refer to symptoms that are psychosomatic that mimic an organic condition. For instance, about a 1/3 of chest pain cases in emergency rooms which appears to be from a heart attack are actually just due to anxiety. About 25% of siezures are psychosomatic, a large % of headaches, and perhaps 40% of lower back pain.
For instance, the RECOVER-NEURO trial tests three treatments - a “goal management training program”, an “online brain training program”, and tDCS. I’m not sure how these trials really are advancing Long COVID treatment in particular — of course someone having cognitive problems might benefit from such things. tDCS is super sketchy — there are no large RCTs showing it work, only hundreds of small studies in low-tier journals.




This smells like research by committee.
Different people, with different opinions about long COVID, came up with a compromise research plan that satisfied everyone.
But it isn't set up to help us crisply distinguish different hypotheses.
A single person, with a single paradigm & hypothesis, whatever it might be, would have come up with a cleaner study.
You really nailed the complexity of this condition!
One reservation I have about such widespread application of medical investigations in the absence of clearly characterised pathophysiology is the danger of over-diagnosis/incidental-findings and subsequent iatrogenic harm. I think this needs to be balanced against the potential benefits of each test.